Peripheral artery disease (PAD) and other forms of vascular narrowing can significantly impair circulation, resulting in pain, fatigue, wounds that don’t heal, and even limb-threatening complications. Fortunately, modern vascular medicine offers advanced, minimally invasive treatments to restore healthy blood flow. One of the most innovative of these is atherectomy—a technique specifically designed to remove plaque buildup directly from the arteries, improving circulation and preventing more serious outcomes.
In this article, we’ll explore what atherectomy is, how it works, who it benefits, and why it’s becoming a go-to solution for restoring vascular health and improving patient outcomes.
What Is Atherectomy?
Atherectomy is a minimally invasive endovascular procedure used to remove atherosclerotic plaque from the inside of arteries. It is typically performed in arteries of the legs, heart, or neck, where plaque buildup—a mixture of cholesterol, calcium, and fibrous tissue—can narrow or block the vessels, impeding blood flow.
Unlike angioplasty or stenting, which compress plaque against the artery walls, atherectomy physically removes the blockage, offering a cleaner path for circulation. It can be used alone or in combination with other interventions like balloon angioplasty or stent placement.
How Atherectomy Works
Atherectomy is performed using specialized catheters inserted through a small incision, typically in the groin or wrist. These catheters are equipped with various cutting, shaving, or vaporizing tools, depending on the type of atherectomy being performed. The procedure is image-guided, often with fluoroscopy, to ensure precision and safety.
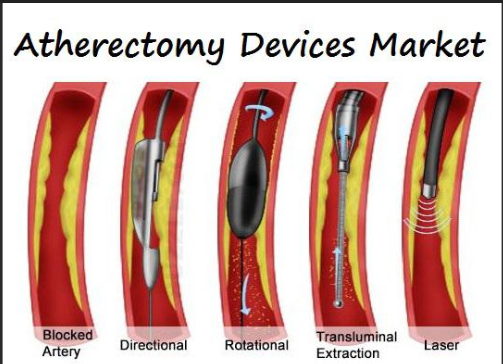
Types of Atherectomy Devices:
- Directional Atherectomy
A small blade cuts and removes plaque in a targeted direction. The plaque is collected in a chamber within the device. - Rotational Atherectomy
A high-speed rotating tip grinds plaque into microscopic particles, which are safely carried away by the bloodstream. - Orbital Atherectomy
Similar to rotational, but uses an eccentrically mounted spinning crown to sand away plaque in a circular motion. - Laser Atherectomy
A laser beam vaporizes plaque through bursts of energy, ideal for softer or mixed-composition blockages.
The choice of device depends on the type, location, and severity of the arterial blockage.

Why Atherectomy Is Performed
Atherectomy is most commonly used in patients with Peripheral Artery Disease (PAD), a condition where arteries, usually in the legs, become narrowed due to plaque buildup. It may also be used in coronary artery disease or carotid artery disease, though less frequently.
Common Symptoms Requiring Atherectomy:
- Leg pain or cramping when walking (claudication)
- Numbness or weakness in limbs
- Non-healing ulcers or sores on the feet or legs
- Coldness in the lower extremities
- Diminished pulses in the legs or feet
- Gangrene or critical limb ischemia
Patients who are not good candidates for bypass surgery or those with heavily calcified lesions may benefit most from atherectomy.
Advantages of Atherectomy
Atherectomy offers several advantages over traditional revascularization procedures like angioplasty or bypass surgery:
1. Plaque Removal
Unlike angioplasty, which compresses the plaque against the arterial wall, atherectomy physically removes the plaque, reducing the risk of recoil or restenosis.
2. Improved Blood Flow
By eliminating the blockage rather than pushing it aside, atherectomy can achieve more effective and lasting improvements in circulation.
3. Minimally Invasive
The procedure is performed through small incisions and typically does not require general anesthesia, resulting in shorter recovery times and fewer complications.
4. Enhanced Results for Stent Placement
In cases where a stent is still necessary, pre-treating the area with atherectomy may allow for better stent expansion and durability.
5. Tailored to Complex Cases
Atherectomy is especially useful for long, calcified, or eccentric lesions that are difficult to treat with angioplasty alone.

What to Expect During the Procedure
The procedure typically takes 1 to 2 hours and is performed in a catheterization lab or an outpatient surgical center.
- Preparation
You may receive a mild sedative and local anesthesia at the insertion site. - Access
A catheter is inserted into an artery, usually in the groin or wrist. - Navigation
Under X-ray guidance, the catheter is advanced to the site of the blockage. - Plaque Removal
The atherectomy device is activated to shave, drill, or vaporize the plaque. - Post-Treatment
Balloon angioplasty or a stent may be placed to keep the artery open. - Recovery
Most patients go home the same day or after a short observation period. Light activity is usually resumed within 24–48 hours.
Risks and Considerations
Although generally safe, atherectomy carries some risks like any medical procedure:
- Bleeding or bruising at the catheter insertion site
- Artery perforation or dissection
- Embolization (plaque debris traveling downstream)
- Infection
- Allergic reaction to contrast dye
Proper imaging, technique, and patient selection help minimize these risks. Your vascular specialist will determine if atherectomy is the safest and most effective approach for your specific condition.
Is Atherectomy Right for You?
Atherectomy is particularly beneficial for patients with:
- Heavily calcified arteries
- Diabetes-related vascular disease
- Critical limb ischemia
- Failed prior angioplasty or stent procedures
- Severe PAD symptoms limiting daily life
If you’ve been diagnosed with peripheral artery disease or have persistent leg pain, sores, or signs of poor circulation, a vascular evaluation can determine if atherectomy or another treatment is appropriate.

Conclusion: A Cutting-Edge Solution for Better Circulation
Atherectomy represents a cutting-edge approach in the treatment of vascular disease, offering patients a less invasive, highly effective method of plaque removal and restored blood flow. Whether used alone or in combination with stenting or angioplasty, this technology provides new hope for individuals facing the daily struggles of poor circulation.
As always, the best treatment plan begins with a thorough consultation. If you’re dealing with PAD symptoms or have been told you need vascular intervention, ask your provider if atherectomy is an option. The right intervention can not only relieve pain but also help you regain mobility, independence, and peace of mind.

